Laura Ng didn’t cry once during nursing school. No tears during her first year and a half of professional nursing, even in an emergency department. But on one of the first days COVID–19 cases started to ramp up, she worked a 16–hour shift: her ER was short–staffed. After getting home, she showered and used the bathroom.
“Then all of a sudden,” she recounts, “it was just full–blown, breathing heavy, sobbing.” In the past, Laura (N’18, GN’21) says, “I haven’t had a huge issue with that crossover of taking work home with me. And it’s been nearly impossible not to in the past month.”
Laura is a nurse in one of New York City’s Mount Sinai Hospitals, at the location where the Upper East Side and East Harlem meet. After graduating from Penn, she worked for a while on an obstetric specialty, but decided to transition to the emergency department to care for ill patients.
On her Thursday and Friday off from work, she visits Brooklyn Fare for a grocery trip after working up the “gumption” to go. She eats popcorn on the couch while watching Bollywood movies. She thinks about her patients, too. The pandemic has made it hard not to.
She thinks about the 38–year old man she calls a “frequent flyer,” who came in often for complications of sickle–cell anemia. He showed up to 1468 Madison Ave, a few blocks from Central Park, one night around 4 a.m..
He’d been staying home, but this seemed serious enough to warrant a visit: he had trouble breathing. And, Laura sighs, “within 45 minutes, we had intubated him and he had died.” His family didn’t even know he was in the hospital.
“You can’t not take that home.”
For Penn Nursing alumni, the novel coronavirus pandemic doesn’t mean they’re staying at home. And for the Nursing Class of 2020, the pandemic means that they’re entering the workforce at an unprecedented time, one that’s redefining the role of nurses in healthcare. Both students and alums are dealing with a tremendous amount of emotional stress and a fundamental tension: this is all part of the job, but it’s not what anyone expected.
Back in Philadelphia, Clare Whitney (N’17, GN’20) is keeping busy. While working at the COVID–19 test site at Citizens Bank Park, Clare would come home, shower off the day’s viral exposure, and work on her dissertation, which she was getting ready to defend via BlueJeans.
Clare’s a member of the Hillman Scholars in Nursing Innovation, an accelerated program that submatriculates students pursuing a Bachelors of Science in Nursing into a Ph.D. program. This isn’t how she pictured finishing out her seven years at Penn. “But,” she laughs, “we’re all just kind of rolling with the punches these days.”
Clare joined the Philadelphia Medical Reserve Corps (MRC) as a volunteer after news of COVID–19 started to spread. It was through the MRC that she started working at the Citizens Bank Park testing site.
A typical shift went like this: arrive in at 11 a.m., get an assignment for a station and a role, head over to meet a team leader. After meeting the team leader and working out a plan, Claire “donned” her PPE. And then the testing site volunteers would work until 6 p.m..
Most shifts, Clare says, she “didn’t use the bathroom or hydrate or eat food because you have to doff all of your PPE as you leave the ‘hot zone.’” Though there’s no rule against taking breaks, she and many other volunteers felt that it was “an ethical choice” to conserve PPE amid the national shortage.
Taking care of herself after work was hard—she’d get home, shower, and do laundry, then set to work on her dissertation again. But, Clare says, “volunteering helped me reckon with my own kind of existential anxiety about this whole pandemic.” It felt good to be useful.
The Citizens Bank testing site closed on April 10, but Clare continued working with the MRC at sites like the Holiday Inn Express in Center City, which has been turned into a site for un–housed people to self–isolate. When she walked to the Holiday Inn from her West Philly apartment, Clare went through the Gayborhood and marveled at the eeriness, the feeling of walking through the streets with no one outside.
Clare’s research focuses on ethics—hospital and clinical. And she’s seen some of these ethical questions move from abstracted to pressing during this pandemic. “One [issue] that makes me reflect on nursing practice as a whole,” she says, “is a lot of the policies that institutions have put in place to keep nurses and other clinicians quiet about the safety issues that they’re facing with limited PPE.”
She’s seen social media posts with people responding to healthcare workers saying, ‘Well, you signed up for this job. Don’t complain.’ But, she counters, “The fact is, we didn't. Nobody signed up to be under these unsafe circumstances. And I don’t mean the pandemic—we did sign up for that—but the PPE shortage.”

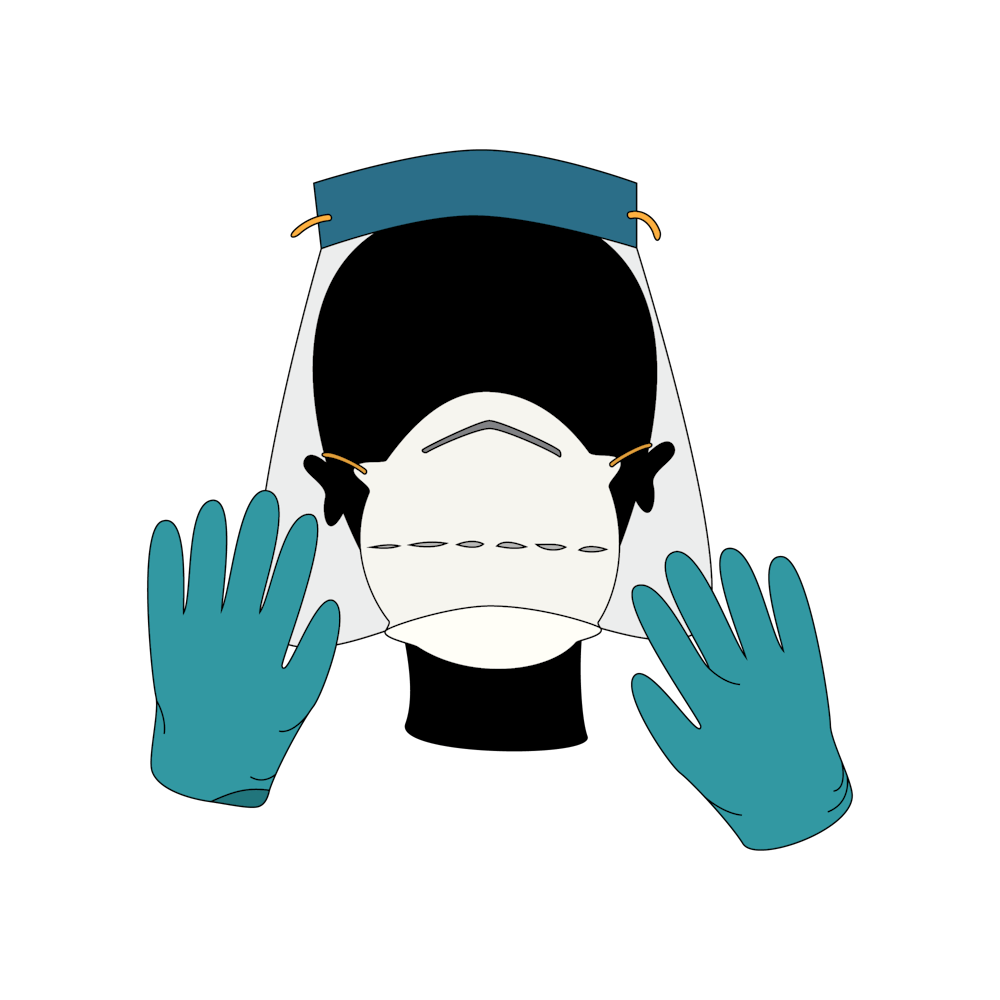
And wearing PPE doesn’t just create a physical barrier; Clare finds it also separates her from patients emotionally. Even as PPE allows nurses to save lives, it also can feel alienating, another stressor that this pandemic has brought to the forefront.
As Clare explains, “the clinical work of nursing is connecting with people. And when you have a face shield and an N95 mask and they can’t tell when you’re smiling, it’s really tough. And so there are a lot of added layers of emotional exhaustion.”
On March 11, Samelle Arhin (N’20) was in Barbados. It was the first Spring Break trip she’d taken with friends, something she’d always wanted to do during college. Then she got that email—the email that announced to Penn affiliates that the school was suspending in–person operations.
“Even though I was in paradise,” she says, “it was very hard for me because the world surrounding me wasn’t matching how my life was unfolding.” Samelle is now back with her parents in Brooklyn, New York, after a flight drenched in Lysol wipes and hand sanitizer.
For current nursing seniors like Samelle as well as Michelle Nigro (N’20) and Gabbie Ramos (N’20), clinicals have moved online and the timeline for licensing exams is up in the air. Post–graduation, they’re figuring out what it means to work in healthcare during a pandemic, or its after–effects: worries about PPE, a lack of clarity on when they can take their exams, and anxiety about the strain on healthcare workers.
In online clinicals, rather than working on hospital floors, they’re evaluating virtual patients: clicking through simulated sepsis rule–outs, performing patient counseling for pixels on–screen.
Michelle understands why nursing students aren’t able to do in–person clinicals. But she wishes she could be doing more. “If you think about it, senior nursing students, we're going to be a nurse very shortly. We have all the skills.”
Gabbie is trying to stay grounded in the day–to–day: studying for exams, finishing out online modules. She watches Holy Week masses on her computer screen and reflects on a year cut short. “There’s a lot of different emotions,” Gabbie says. “It’s just so much uncertainty and it really does force you, I think, to live in the present more than ever. Because they could change a policy tomorrow.”
Michelle is slated to start work at Johns Hopkins in August, on a neuroscience floor. She says she hopes to take the NCLEX, the licensing exam for registered nurses, in July, but worries that it might be pushed back. Gabbie’s been looking for jobs and may find one that requires a Temporary Practice Permit (TPP), which allows nurses to practice if they’ve graduated from nursing school but haven’t yet gotten their state board licensing exam done.
In response to the coronavirus crisis, the NCLEX has changed some of its requirements: shortening the exam, limited testing slots to maintain social distancing, and closing some test centers. Gabbie says that Penn Nursing faculty have advised her to apply for a TPP to practice in Pennsylvania, which she can only do after graduation. Processing a TPP can take up to 70 days, and faculty have also told her that it will likely take longer than usual to get licensed. As a result of these changes, many members of Nursing’s class of 2020 are unsure when they can enter the workforce.
And once they get there, the field that 2020 Nursing graduates are entering will look different from any time in recent memory. Samelle adds that whenever she’s able to start work, “the repercussions of COVID are still going to be very real.” She continues: “it’s sort of like 9/11—it’s going to be something that people lived through and were affected by, whether directly or indirectly. And that’s going to influence the care I give to people.”
All of these nursing students, as well as Clare and Laura, speak about the emotional toll of preparing to work in healthcare under the storm clouds of a pandemic. When the University of Pennsylvania Health System (UPHS) sent out an email on April 1 to put together a list of students willing to volunteer in UPHS hospitals, Gabbie thought about what it would mean to start hospital work now.
“As invincible as you feel as a young person, a college student, someone starting nursing, then you see all these people who are not the typical at–risk for death by COVID, people getting very sick or even dying. And when you see that it’s definitely, it’s like tension in your heart,” she says.
“I want to help, I want to be on the front lines and I feel called to nursing and I signed up for this. But also, maybe I'll just stay at home right now until I have my license and actually go in then.” Gabbie did sign up to volunteer, despite worries about potentially having to self–isolate from her family, but hasn’t heard anything back.
But that tension doesn’t go away—it gets deferred to after graduation when she and other 2020 graduates may face COVID floors and continued PPE shortages. Some members of Michelle’s family tell her they’re glad she’s not working now—and she gets where they’re coming from. “If it was my kid,” she says, “I’d be worried.”

Gabbie worries about what happens when she does go to work, when “you’re probably going to start wearing an N95 mask and a face shield everyday, and just living with this level of anxiety being in the healthcare field as a new nurse.” She and the rest of the class of 2020 will be learning how to be a nurse outside the classroom, “still supported but now…held to this higher level of accountability.”
And on top of that, Gabbie adds, they’ll still “have to worry about all this COVID chaos and new protocol nonstop.”
These students also know that nursing isn’t just about direct patient care, and that worries about PPE and getting sick don’t encompass the full weight of the job. For Samelle, Michelle, and Gabbie, as well as the rest of the graduating class of nurses, there’s an anxiety about dealing with a range of responsibilities—care, advocacy, and emotional labor, especially during a pandemic—on top of the anxieties that nurses face every year about graduation and starting to practice as a professional nurse.
“The thing about nursing,” Samelle says, “is that it encompasses a whole bunch of other careers all in one. You feel like you are a grief counselor. You're a therapist, you're a lawyer in that you advocate for your patients and like you are even a spiritual person as well, depending on the cultural and religious beliefs of your patients.”
“Nursing gives you the opportunity to be many things for a patient in their most vulnerable time.”
These nurses and nursing students appreciate the attention paid to healthcare workers during this pandemic. But they also realize that it’s fleeting, or that it may not address deeper problems.
There’s the mental weight of being the last person a patient sees before they die. There’s the worry about being separated from that patient only by layers of dwindling PPE. There’s the gratitude of being called heroes and thanked for their work, but also the knowledge that any day in the ER or at a testing site is fundamentally another day at work.
Samelle says, “COVID has just shown me that although nurses are essential workers, we’re not always going to be cared for in the same way we care for others.” She’s grateful to God, she says, “for all of the congratulatory and reactive responses of gratitude that people have shown.”
But “nurses have always been nurses. Now they’re just being seen in a different way.” And, she says, emphatic, “I still think it’s important that the protective care is there, that our president is caring about us.”
Laura says of “the whole calling people in healthcare heroes” thing, that “it's nice to be appreciated, but it feels very strange because to me, my job, of course there's differences in it, but fundamentally it's not that different.”
She continues: “my routine has, in some ways, been massively disrupted, and in some ways it hasn't been disrupted at all.”
According to Laura, the best way to support nurses is to care for communities bearing the brunt of coronavirus. She’s seen firsthand the disparities in care for wealthier and poorer communities. Working on the border of the Upper East Side to the South and East Harlem to the North, she says, makes her realize that it’s great for healthcare workers to get a free lunch, but it’s more important to care for vulnerable communities, and not just during this pandemic.
In the future, she hopes that this pandemic will galvanize some sort of action to help disadvantaged communities, which will in turn help lessen the load on the healthcare system. “I hope we can use this efficiently to help the people who have always needed it most. I don't think any of us—at least from the people I know—no one wants to be commemorated as like a hero…What we need is for people to pay attention to these at–risk populations, because that's what's going to help us the most.”
Clare recently defended her dissertation from her West Philly apartment, where she’s isolating alone. Before a close friend—and another Hillman Scholar—left Philadelphia to isolate with family in Baltimore, she dropped off some canned goods at Clare’s door. She also left a bottle of champagne with a label: “for defense.” Claire says, “I’ll still be celebrating, just remotely.”
And in a few weeks, Samelle, Gabbie and Michelle will graduate from the School of Nursing on May 18. They’ll stream commencement from computer screens rather than sitting on Franklin Field.
People keep asking Gabbie if she’s upset that graduation and commencement are cancelled. “Trust me,” she says, “I wanted to be there with my friends and celebrate all the hard work we put in.” But she’s okay. “In my heart, I know I have already had moments of pride and love and joy and fulfillment that are way more than a three–second walk across a stage will ever be.”
And Laura will keep going to work. At her ER, the week of April 16 was the first week when, she says, they’ve seen the fervor of coronavirus cases slow down. It’s anecdotal, but it’s a good sign. As she recounts the good news, she knocks on wood. The sound echoes through the phone.

The weirdest part about all of this, Laura says, is the culture shock. Simply put, she’s not used to seeing this many people die. That’s what her colleagues in the Intensive Care Unit go through all the time. “Kudos to them. I don’t know how they do it,” she says wryly. Ordinarily in the ER, she’s trying to stabilize patients, and seeing deaths mainly when they’re unresponsive to CPR.
It’s hard to see people dying like that, “especially without family or friends, and knowing that we’re what they have,” Laura says.
“And we’re busy. We don’t have time to sit there and hold their hands. Because we have other patients who are going to follow in their same footsteps if we don’t care for them.” So it’s back to intake and IVs and intubations. It’s a pandemic, but she can’t afford to slow down, because it’s also another day on the job.